What is Juvenile Idiopathic Arthritis?
Juvenile Idiopathic Arthritis (JIA) is a general name for several kinds of arthritis. “Juvenile” means that it affects young people, “idiopathic” means that we don’t know what the cause is, and “arthritis” means inflammation of the joints. Juvenile Idiopathic Arthritis used to be called Juvenile Chronic Arthritis (JCA). In some countries it is called Juvenile Rheumatoid Arthritis (JRA), and sometimes people simply call it Juvenile Arthritis (JA).
JIA is chronic arthritis that begins in children under 16 years of age. It causes inflammation in one or more joints for 6 weeks or longer.
JIA can appear in many different ways and can range in severity. It mostly affects the joints and the surrounding tissues, although it can affect other organs like the eyes. Some of the symptoms and signs of an inflamed joint include joint swelling, pain, stiffness (especially in the morning), and warmth around the joint. Your child may not have all of these in every joint that is inflamed. Less commonly, your child may also have other symptoms such as fever, rash, loss of appetite and loss of weight.
What does chronic mean?
- painful, swollen or stiff joint(s)
- joint(s) that are warm to touch
- increased tiredness
- a fever that keeps returning
- a limp but no injury.
Conditions can be acute (starting suddenly or short-lived) or chronic (lasting longer but not necessarily forever). JIA is considered a chronic condition because the joints involved are inflamed for at least 6 weeks and while treatment can alleviate the symptoms it does not lead to a ‘cure’. This means that when a child is diagnosed with JIA, it is impossible to say exactly how long the condition will last. JIA can continue for months or years. Sometimes the symptoms go away, usually after treatment. This is called remission. Remission may last for months, years, or for a lifetime. Up to 50% of children with JIA may go into full remission before adulthood.
How common is JIA?
JIA affects at least one child in every 1,000 in Australia. There are at least 5,000 children in Australia with JIA.
This information sheet is about Juvenile Idiopathic Arthritis (JIA), its cause, treatment and what it may mean for your child and your family.
Hearing that your child has JIA can be a shock because people think that arthritis is a condition that only affects older people. You may feel overwhelmed by the diagnosis of JIA. This is normal – there are lots of things to think about. You will probably have many questions. You may like to make a list of questions to ask your child’s rheumatologist or rheumatology nurse educator at your next appointment. You may need to hear the answers several times. That’s OK. It is important for you and your child to know about JIA.
What causes JIA?
We do not know the causes of JIA. However, we do know it is an auto-immune condition. Our bodies have an immune system which fights germs or viruses to keep us healthy. Sometimes the body’s immune system mistakes a normal part of the body for something foreign (like a germ), and starts attacking the body itself. In JIA the immune system attacks the joints. This is called an auto-immune process. We don’t understand precisely how, or why this happens.
JIA is not hereditary – it is not passed on from parent to child. It is rare for two children in the same family to have JIA, although this can happen. Genes do play a role, but are only one of a number of factors necessary to develop JIA.
Having JIA is no one’s fault. There is nothing that anyone has done, or not done that caused JIA. There are myths that JIA is caused by being too cold, by living in a cold climate or eating particular foods. None of these actually contribute to a child getting JIA.
What are the different types of JIA?
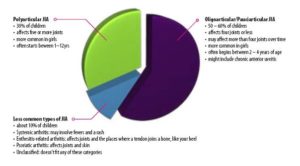
All types of JIA cause inflammation in the joints and begin before the age of 16. The different types of JIA are defined by the number of joints that are inflamed in the first six months, and by other symptoms that might be present. (Acknowledgement: Royal Children’s Hospital/ Rheumatology website).
How is JIA diagnosed?
JIA can appear like other childhood illnesses and can be different from one child to the next so your child’s doctor will ask many questions and perform a medical examination of your child. The doctor may order some of the following tests.
• Blood tests which look for inflammation CRP, ESR; full blood count (FBC); autoantibodies; electrolytes; liver and kidney function; HLA-B27 (genetic marker); Rheumatoid Factor (RF) Cyclic Citrullinated Peptide (CCP);
• X-Rays; ultrasound, CT Scan, MRI, Bone Scan
• Electrocardiogram (ECG) to check your child’s heart
• Joint aspiration
• Bone marrow aspirate (but this is less common)
There is no one test to diagnose JIA. It can be hard for families and their child to cope with the uncertainty of a diagnosis.
Health Care Team
A range of healthcare professionals may be involved in helping your child with JIA and your family manage the arthritis:
- Child and their family
- GP
- Paediatric Rheumatologist
- Rheumatology Nurse
- Physiotherapist (Physio)
- Occupational Therapist (OT)
- Dietitian
- Ophthalmologist/ Optometrist
- Counsellor/ Psychiatrist/ Psychologist
- Pharmacist
- Podiatrist
- Dentist
- Teachers
- Support Group
Treatment for JIA
JIA is different for each child, so their treatment will need to be tailored to their specific needs. Finding the right treatment for your child with JIA may take time, involve trialling different therapies, have to be altered if the JIA progresses or flares.
The goals of treatment are:
- to reduce inflammation
- to reduce pain (usually due to inflammation)
- to prevent (or slow down) the damage to joints
- to make sure joints keep working as best they can
- to get your child back to their normal activities and to prevent arthritis from interfering with a full and active lifestyle.
The main treatments for arthritis include:
- medications to control the inflammation (including tablets, injections, infusions, eye drops)
- exercises to keep the joints moving well and the muscles strong
- splints to support the joints
- joint injections to reduce inflammation in particular joints
- pain management strategies to reduce pain and to help your child cope with pain
(Acknowledgement: Royal Children’s Hospital/ Rheumatology website)
Medications for JIA
There are many medications used to treat JIA. The doctor may prescribe a non-steroidal anti-inflammatory (NSAID) first and if the JIA is not well controlled another medication may be prescribed such as a corticosteroid, disease modifying anti-rheumatoid drug (DMARD) or biologic. Sometimes children require a combination of these medications to keep their JIA under control. Pain relief (analgesic) medication(s) may also be required. It is important not to stop any of these medications without first contacting the doctor.
For more detailed information on each medication follow the links below:
Anakinra (Kineret)
Azathioprine (Imuran, Azamun, Azapin)
Cyclophosphamide (Cycloblastin, Endoxan)
Etanercept (Enbrel)
Hydroxychloroquine (Plaquenil)
Leflunomide (Arava, Arabloc)
Methotrexate ( Methoblastin)
Methotrexate- Parent Information
Subcutaneous Methotrexate- Parent Information
Mycophenolate mofetil (Cellcept, Myfortec)
NSAIDs ( Nurofen, Brufen, Celebrex, Naprosyn, Orudis, Voltaren)
Paracetamol (Panadol, Panamax, Panadol Osteo)
Prednisolone, Prednisone (Panafcort, Panafcortelone, Predsone, Predsolone, Solone, Sone)
Sulfasalazine ( Salazopyrin)
Five Ways to Get Kids to Stick to Their Treatment Plans
Follow these tips to help your child stick with the prescribed JIA therapy program.
Getting kids to take their medication or do their exercises can be a tricky task. Here are some rules to remember:
- Routine – make it a habit for your child to do her exercises or take her medications. Set aside the same time every day or week as necessary.
- Reward your child with age-appropriate and goal-appropriate prizes for sticking to their treatment plan. Dinner out, a trip to the roller skating rink or a box of crayons can all have their place in a reward system based on accumulating points over days and weeks.
- Reassure your child that taking her medication makes a big difference in how she feels. It may not change how she feels today but it will make a difference in a few days, weeks or years.
- Relinquish control when your child is ready to take his medications on his own. Letting a responsible teen be in charge of his medications, while still reasonably monitoring him, helps him take responsibility for his health in the long run.
- Remind your child when needed. Everyone needs a little reminder every now and then. Your commitment to your child’s treatment plan is as important as hers. But when you remind, make it a positive encouragement; avoid nagging.
(Acknowledgement: Kids Get Arthritis Too website)
Joint Injections
Joint injections reduce inflammation and pain in swollen joints. If you only have a few swollen joints they may be the only therapy you need. If a child with JIA is on medicines already and still has swollen joints, joint injections may save having to increase their doses or change them.
Steroid injections are performed in a hospital clinic or day surgery unit. Local anaesthetic cream, “laughing gas”, sedatives or general anaesthetics are used.
The doctor will insert a needle into a joint to remove some fluid, and then inject the steroids. Most children notice that the joint is a lot less sore and swollen within a few days after the injection. Injections can make joints feel better for weeks, months or even longer.
Uveitis
Uveitis is inflammation that occurs in the eye. Inflammation is normally one of the body’s protective responses to infection or injury, but in diseases such as uveitis, uncontrolled inflammation can cause damage. Uveitis is the most common eye problem associated with juvenile idiopathic arthritis (JIA). Uveitis is more common in children who have a positive anti-nuclear antibody (ANA)
There are different kinds of uveitis associated with JIA. The most common form of uveitis has no symptoms (‘silent uveitis’), which is why regular eye check-ups are essential. However, your child may complain of blurring of vision, sensitivity to light, and rarely, eye redness or pain. If left untreated, uveitis can result in loss of vision.
As there may be no symptoms, all children with JIA need to be regularly assessed by an ophthalmologist (specialist eye doctor). The ophthalmologist will look into the back of your child’s eyes with a special microscope called a slit lamp. Some children may be assessed by an optometrist, particularly older children (e.g. over 8 years of age). How often each child needs to be seen will be decided by their ophthalmologist or optometrist. For children without uveitis they may be seen initially every three months then over time this may extend to less often (e.g. six monthly). Children with active uveitis may need to be seen much more often by an ophthalmologist but your child’s doctor will direct this plan.
If uveitis occurs, the ophthalmologist and rheumatologist will work together to treat your child to prevent permanent eye damage. Treatment may require steroid eye drops. Sometimes other eye drops are required. If the eye drops don’t control the uveitis or the uveitis is severe, your child may require other medicines by mouth or injection. (Acknowledgement: Arthritis Australia information sheet JIA/ Uveitis)
Diet and JIA
There is no one special diet that has been shown to be effective for arthritis.
Very few diets or foods have been tested in a scientific way. The usual recommendation for a child with rheumatic disease is that they eat a standard balanced diet. However certain foods and oils have anti-inflammatory and antioxidant properties. These include:
- Olive oil
- Fish that are high in omega-3 such as salmon, tuna, mackerel
- Fruits and vegetables, especially red and purple fruits such as cherries, strawberries, blueberries
- Vitamin K-rich veggies like broccoli, spinach, lettuce, kale
- Vitamin C-rich citrus fruits
- Nuts such as walnuts, pine nuts, pistachios and almonds
- Beans, such as pinto, black, red kidney and garbanzo
If corticosteroids are a part of your child’s medications, then it is important to limit the dietary intake of fats and sodium and to make sure they get enough calcium in the diet or combination of diet and calcium supplements. Your child’s doctor will advise on whether these need to be taken.
Does a gluten free diet have any impact on JIA? Having one autoimmune disorder increases the likelihood of having another. Coeliac disease is an autoimmune disorder. A gluten free diet is a medical necessity if a child has diagnosed coeliac disease. Talk to the doctor or dietitian if you are concerned your child has coeliac disease or gluten sensitivity.
(Acknowledgement: Kids get Arthritis Too, US Website)
Exercise
Regular daily exercise is important in maintaining muscle and bone strength, reducing pain, increasing energy levels, reducing joint stiffness, anxiety and improve sleep at night. Children with JIA should select activities they enjoy and that they can do with their friends and family. Types of exercise:
Range of Motion– helps to reduce stiffness and improve joint motion. Most effective if done daily but may be hard to maintain. Child can chose which ROM exercises work best on the stiffest joints and do them as often as possible. Doing the ROM exercises in the shower may be easier and are gentle enough to do even when joints are painful or swollen.
Stretching– Stretching can reduce stiffness and help keep joints and muscles flexible. This can make everyday activities much easier. Stretching gradually expands range of motion by improving muscle flexibility. Stretching can also help a child to move more comfortably. Should be done after a 5-10 min warm up, 3-4 times per week, after a shower can help, done slowly and held for 20 seconds.
Strengthening – Strengthening muscles help support joints, which is very important for children with JIA. Isometric is exercising without moving the joint. Isotonic exercises are exercises that involve moving the joint and resistance can be added using body weight, elastic exercise bands or weights. Resistance can be added if you can complete two sets of 10 repetitions of an exercise easily, you can add some resistance. You and your child may be feeling overwhelmed by all of the exercises that you have been given. Talk to the physiotherapist about how to make this more realistic.
Cardiovascular fitness– The ability of the body to do an activity like swimming or walking for an extended period. It can help maintain a healthy weight, help control pain, and improve sleep and mood. Any continuous activity will help. Swimming, water aerobics, hydrotherapy, brisk walking, in-line skating, dancing and cycling may be easier to do for children who have JIA.
Note: Can participate in impact activities and competitive contact sports if their disease is well controlled and they have adequate physical capacity.
Physiotherapy: physiotherapists can provide an individualised exercise plan to maintain joint function, avoid exercise related injury and splinting or mobility aids. This plan might include hydrotherapy/ aquatic physiotherapy, taping, massage, splints, heat or ice packs and dry needling.
Splints
Splints may be suggested for various reasons, such as to rest the joint and reduce pain or to correctly position the joints to prevent deformity and improve function. Can be ready-made from soft, flexible material such as neoprene, or tailor-made by the occupational therapist (OT)or physiotherapist from a type of plastic to specifically fit your child’s joint(s).
Resting splints worn at night hold the joint in a good position. This helps with posture and use of the joint. Working splints are worn during the day to maintain position, function and pain during daytime activities.
Orthotics or shoe inserts may help with differences in leg length or balance problems. A podiatrist can assess gait and measure, cast, fit orthotic devices. (Acknowledgement: Versus Arthritis, UK website)
Fatigue and Pacing
Children with active disease, especially those experiencing flares, are more likely to feel fatigued.
- chronic inflammation from active JIA and its effects on the body may produce fatigue
- pain also causes fatigue
- Chronic Fatigue Syndrome and Fibromyalgia are other conditions, which cause constant extreme fatigue
- inflammation caused by JIA can affect how the body processes iron leading to iron deficiency (anaemia) and fatigue
- some medications can cause fatigue
- emotional health issues can cause fatigue
Children who do not have active JIA can still have chronic pain if their joints are damaged which is more likely to be causing their fatigue than the inflammation process.
How can you and your child pace their activities?
Take control. Changing medications or using nondrug therapies may help better control your child’s pain and inflammation, two of the most common fatigue triggers. Talk with your child’s doctor about options. Also, you should also check if your child has another health condition that causes ongoing tiredness.
Sleep well. JIA can affect sleep quality, so encourage your child to practice good sleep hygiene. This includes sticking to a regular sleep schedule, avoiding caffeine before bedtime, and creating a relaxing bedtime routine (for example, warm showers or baths, reading, listening to relaxing music).
Get moving. Exercise gives you more energy, stamina, stronger muscles and can improve sleep. Studies in adults show that increasing activity improves fatigue. Walking, biking or swimming are great options. Your child’s rheumatologist or a physiotherapist can suggest other activities.
Stop stressing. Stress at school or at home can cause fatigue and poor sleep, and clinical depression is much more likely in children with JA. A therapist or psychologist can suggest ways to relieve anxiety.
Eat smart. A nutritious diet can help your child maintain a healthy weight. If your child is a picky eater or has a sugary diet of processed foods, they may not be getting the nutrition they need. Your doctor or a registered dietitian can help you figure out what your child’s diet may be lacking, like iron to prevent anaemia.
There is no one-size-fits-all way to manage fatigue. Working with your child and his doctor to find the possible causes is the first step.
(Acknowledgement: Kids Get Arthritis Too, US Website)
How can JIA pain be managed?
Many factors may influence the onset and persistence of musculoskeletal pain in children with JIA: poor sleep; fatigue; unhealthy diet; low mood; inactivity; site of pain; disease activity and severity; your child’s coping ability; previous experience with pain or illness; lack of support from others; medications not working; stress to name a few.
Things your child and you can do to manage pain:
- Use relaxation techniques: deep breathing
- Yoga and stretching
- Mindfulness
- Heat and cold (warm bath or shower, heat or cold packs wrapped in a cloth, wheat packs)
- Regular pain medications as prescribed by your child’s doctor (try not to miss or skip doses)
- Hydrotherapy (a program by Physio or exercise physiologist should be obtained to ensure exercises are appropriate)
- Gentle regular exercise as advised by doctor or physio
- Distraction (listening to music, watching video, playing a board game, reading, an activity your child enjoys)
If you or your child are finding it hard to manage, seek help from a counsellor, psychologist or talk to your child’s doctor about a referral to a Pain Management Unit (PMU) or pain specialist. For children living in the ACT a doctor’s referral to the PMU Westmead or Randwick in Sydney could be considered. If your child sees a rheumatologist in Sydney then they will refer as required.
(Acknowledgement: National Rheumatoid Arthritis Society NRAS, UK website)
Seven Tips for Managing Your Child’s Arthritis Flares
Find out how you can help your ease your child’s pain during a flare.
A flare is the term for that period of time when your child’s juvenile arthritis is more active. She may not feel well overall, she may have joint pain or her joints may be swollen, pink or stiff. Here are a few ways you can help your child through a flare:
- Make sure your child takes medicine on time – often flares are the result of missed dosages.
- Call your child’s doctor if you suspect your child is having a flare.
- Apply ice to sore joints for 20 minutes at a time with 10 minute breaks.
- After the first 24 hours, heat may be soothing for sore joints. Ask the doctor to teach you massage for achy joints.
- Change your child’s activities so they are easier to do when they are in pain.
- Keep your child active to keep up their muscle strength and flexibility.
- Ask your child’s doctor about using splints at night. Splints can prevent joints from moving around and causing more pain.
(Acknowledgement: Kids Get Arthritis Too website)
How can parents support their child with JIA?
- Being sympathetic and understanding of the difficulties your child is going through is very important.
- As early as possible involve your child in their treatment, to encourage independence and a sense of control.
- Discuss any issues with the health care team.
- Write down questions you have and take them to the next appointment with the health care team.
- It’s important to take care of your own well-being too. As a parent, it can be a worrying time, so don’t be afraid of discussing your worries with people you trust.
- Learn as much as you can about JIA.
- Talk about thoughts and feelings.
- Talk about your child’s condition and management of their healthcare with the whole family and face it together.
- Like school, hobbies such as sports, music and other activities should be continued to give your child as normal a routine as possible.
- It’s sensible to maintain rules around behaviours which a child/young person can control and to keep life as normal as possible when they’re well. Special treats/allowing certain behaviours when unwell sometimes need to be stopped when well.
- Plan social activities that the family enjoy together.
- It can also be helpful to talk to another family who’ve been through the same experience.
Support for your child with JIA and your family.
Meeting other families who have a child with JIA can be a valuable experience for your whole family. It can help to share ideas and experiences with other families in the same situation. Local Arthritis Foundations often run support groups for parents and activities for families. Arthritis ACT has a Facebook Group called Canberra JIA Support Group, to join request via Facebook or email info@arthritisact.org.au
Arthritis and Osteoporosis NSW offer JIA camps annually:
Twinkletoes camp for under 8yrs of age Camp Twinkletoes for under 8yr olds with JIA
Footloose for kids with JIA from 9-18yrs of age Camp Footloose for 9-18yr olds with JIA
How can grandparents, relatives or friends help?
- When offering help, be honest about things you feel able to do.
- Keep offering help – things change and the family may suddenly need help where they didn’t before.
- Be led by parents – they will tell you what they need.
- Listen to parents when they need to let off steam. This is normal, and you are a safe and supportive person they can talk to.
- Just be there.
- Share information you find about local support groups and services. However, make sure that the information is correct and comes from a reliable expert source.
- Prepare a meal for the family that can be frozen and used when needed.
- Write a card or send flowers to show you are thinking of them.
- Offer to help with the garden, shopping, or fetching prescriptions or medicines.
- Offer to accompany the child and parent to different appointments. Help with transport and parents value moral support.
- Offer to babysit. Each child will value having special time with you. Both the child with JIA and their healthy siblings need to feel special every now and again.
- If it is appropriate, you could offer to stay at the family home and mind the children while the parents have a night away. This is less disruptive to the children’s normal routine and allows easier access to any special equipment.
(Acknowledgements: Royal Children’s Hospital/ Rheumatology website and Choices for Families of Children with Arthritis, 2003)
School: Information for parents
In the ACT most schools offer an Individualised Learning Plan (ILP) for any student with learning needs. This is a plan developed between, the student, parents and teachers. Proof of diagnosis and any disabilities need to be provided, reports or letters from your child’s doctor, specialist, physiotherapist, occupational therapy, psychologist/ psychiatrist for example. If your child’s needs meet certain criteria required by the ACT Education Directorate or Catholic Education Office the school can obtain extra funding to help with your child’s education.
An occupational therapy assessment done at your child’s school may help with educating teachers, having equipment tailored to your child’s needs and a more inclusive ILP.
The NDIS generally do not fund equipment or supports for your child’s schooling. School supports should be discussed with your child’s school.
Other things that might help:
- Shorter days at school, late starts and attending just the core subjects.
- Pacing activities at school, using a pedometer to count steps, lift pass.
- Help children learn to problem-solve and become confident in managing JIA by discussing difficulties they have had during the day, and suggesting strategies they could use to help.
- Home schooling may be an option or part home schooling and attendance at a school may be an option.
- Talk about thoughts and feelings.
- Talk about how to build friendships and deal with social difficulties.
- Encourage social activities with your child’s friends and classmates.
- Trial mobility aids at your child’s current school or if moving to a new school.
- Work with your child’s teacher in educating their classmates about JIA.
- ICT may help your child stay connected with their school and class so they feel less isolated.
- Voice to text software to help reduce typing or writing fatigue.
- Regular meetings with your child’s teacher(s) to remain up to date with schoolwork and provide you with information on what can be done at home when your child is unable to go to school.
- Provide a treatment or action plan to your child’s school for any treatment that is not basic first aid. Such as pain management plan, asthma action plan.
Provide required medications and instructions for administration, with a doctor’s letter to be kept at the front office or sickbay.
School: Information for teachers
There may times when the arthritis gets better or worse which is called a ‘flare’ or ‘flare-up’. This is important for teachers to know about this, generally on a bad day a child with JIA will not attend school. A child’s physical abilities, pain and mood can change from day to day. The child and their parents about what should guide teachers, how much and when they can do at any particular time. Children often will hide or ignore their symptoms in order to fit in with their peers than overplay their symptoms in order to avoid activities.
How can teachers help?
- Let the child know it is OK to move about when they need to do so.
- Make a plan with the student about how they can move regularly in the classroom.
- Arrange for extra time or rest periods during activities where there is a time limit.
- Provide extra explanations for tasks, homework, assignments, missed work particularly if the student has been absent from school.
- Alternate passive and active activities over the school day.
- Monitor the student for signs of fatigue. Older students may be able to have a hall pass to leave the classroom to go for a rest at a designated area.
- Provide accessible seating: in assembly, the student may need to sit on a chair not the floor.
- Appropriate seating: ankles and knees are at 90-degree angle and hips are at 70-90 degree angle. Base of the chair should not slope backwards. Student should be able to rest their feet on the floor. Desk should be just above elbow height when sitting.
- Use of grip pens, It device such as laptop, iPad, keyboard.
- Allow adequate time for student to move form area to another.
- Two sets of textbooks or ability to leave class books in the classroom.
- Educate other students about JIA in partnership with the student who has JIA.
- Student may need to attend for shorter days or start later.
- Keep the student up to date with what has been happening at school.
For a more detailed list of ways to help a student with JIA refer to the information sheet section below. (Acknowledgement: RCH and APRG* rheumatology resources for patients and families)
Information Sheets
What is Juvenile Idiopathic Arthritis?
Finding out your child has JIA booklet
What are the different types of JIA?
Treatments Commonly Used for JIA
Managing the impact of JIA on your Child’s life
Managing the impact of JIA on your Family’s life
Physical Activity and Arthritis
Emotional Well Being and Arthritis
Good Sleep Habits
Breathing and Relaxation Strategies
Young People living with Arthritis
JIA information for sports teachers
Information Sheets on other conditions
Anterior knee pain
Bechets Disease
Chilblains
Chronic Recurrent Multifocal Osteomyelitis (CRMO)
Familial Mediterranean fever (FMF)
Growing Pains (Benign nocturnal limb pains (BNLP)
Hypermobility Syndromes
Juvenile Dermatomyositis (JDM)
Localised Scleroderma
Osgood Schlatter
Sever’s Disease
Links:
Autoimmune Resource and Research Centre
Australian Rheumatology Association
Kids Get Arthritis Too (Arthritis Foundation, US)
Paediatric Rheumatology InterNational Trials Organisation (PRINTO)
Royal Children’s Hospital, Melbourne
Sydney Children’s Hospital Randwick
Sydney Children’s Hospital Westmead
Social Media and Support Links:
Kids Arthritis Family Support Group
Musculoskeletal Australia’s Kids Facebook Page
Canberra JIA Support Group closed Facebook group, to join contact info@artritisact,org.au
Kids Get Arthritis Too- meet other families
Kids Get Arthritis Too, info for kids
Kids Get Arthritis Too, info for teens
Olivia’s Vision- Info and support on Uveitis
Apps:
Versus Arthritis, UK- symptom tracker for teens app
Other:
Taking Arthritis to School written by Dee Dee Miller
If you need further information about Juvenile Idiopathic Arthritis, please call us on free call 1800 011 041.





